 This Term’s Christmas Blurbs highlighted Neuroscience - a field that is strongly represented in Brasenose’s research community. Two presentations, one by a graduate student and one by a tutor, demonstrated how investigations into brain circuitry is helping to develop new treatments for epilepsy and Parkinson’s disease.
This Term’s Christmas Blurbs highlighted Neuroscience - a field that is strongly represented in Brasenose’s research community. Two presentations, one by a graduate student and one by a tutor, demonstrated how investigations into brain circuitry is helping to develop new treatments for epilepsy and Parkinson’s disease.
John Jefferys (Professor of Neuroscience, Department of Pharmacology) launched proceedings. Just under 1% of the population has epilepsy. Professor Jefferys described three common types of epilepsy: a generalised seizure (sometimes described as an epileptic fit), an absence seizure (or blanking out), and a complex partial seizure. Professor Jefferys’ team are researching the latter condition. While many individuals are able to live comfortably with epilepsy, there are unfortunately around 1,000 deaths per year in the UK causally linked to the disease. Approximately 400 deaths occur as a result of accidents while 600 are attributable to SUDEP (sudden unexplained death in epilepsy). Although mortality is relatively low, each death has a devastating impact on the family and friends of the deceased. Professor Jefferys’ group is exploring the links between excessive brain activity and abnormal heartbeat.
The brain is wired to the heart via two systems: the sympathetic and parasympathetic nervous systems. Cells along these tiny pathways of nerves pass on electrical signals that either accelerate or dampen the rate of heart beat. Epileptic episodes trigger abnormally fast and irregular cardiac rate and rhythm. One immediate consequence can be a blackout since the efficiency with which oxygen is supplied to the brain deteriorates, leading to temporary loss of consciousness. Professor Jefferys’ group are looking at potential longer-term degradation of heart tissue resulting from repeated seizures with the aim of developing drug treatments capable of mitigating these impacts.
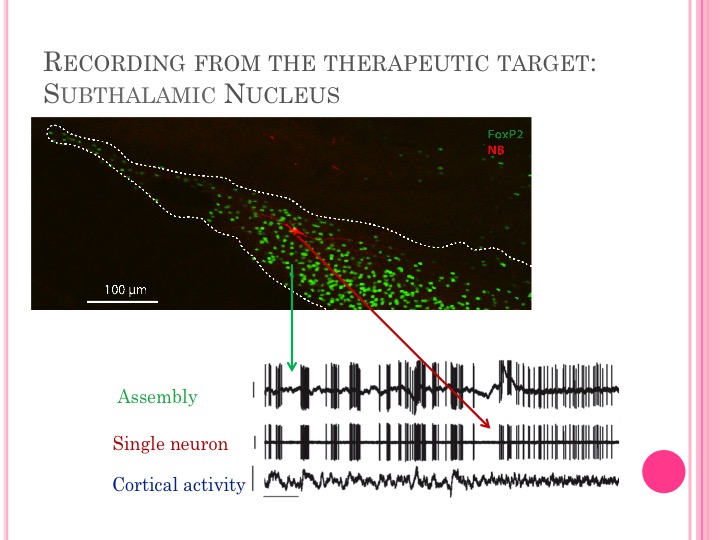
Neuroscience studies brainwaves which are synchronised electrical pulses created by the interaction of millions of neurons. In a healthy brain, these oscillations are rhythmical but if the pulses become irregular medical problems can result. 2nd year DPhil student Eszter Kormann started her blurb by referring to abnormal oscillations as a ‘fingerprint of the disease’. Her research examines the link between Parkinson’s disease and beta oscillations, caused by disrupted dopamine transmission in the brain’s basal ganglia region. Dopamine acts as a fuel for firing neurons and its depletion disrupts the communication of ‘stop’ and ‘go’ signals transmitted to the cortex, resulting in a slowing of movement, gait disturbances, and trembling - characteristic symptoms of Parkinson’s.
One treatment, called deep brain stimulation, relies on the chronic implementation of an electrode into the patient’s subthalamic nucleus (part of the basal ganglia). The electrode is attached to a pacemaker that can deliver continuous stimulation to generate improved neural signalling. The surgery can be dangerous to perform and stimulation is currently limited by significant side-effects and the fact that it’s not applicable to all patients. Eszter is part of a group investigating an alternative treatment called phase cancellation. Delivering the anti-phase of the pathological oscillation can, in theory, facilitate the reduction of beta oscillation, leading to improvement in the motor symptoms.
Both presenters acknowledged the role that experimentation on laboratory rats plays in their respective research projects. Animal experiments must be licensed by the Home Office which imposes strict controls, recognising the ethical concerns associated with vivisection. Lab rats are used for several important reasons. Human trials have limitations in terms of not having the experimental flexibility and controls due to ethical implications. Removing tissue samples from a patient’s brain to examine the impact of interventions on cells (plasticity effects) is also not always possible.
Read Eszther's blog here.
